Cancer’s Secret Safety Net
Researchers uncover a hidden mechanism that allows cancer to develop aggressive mutations.
Researchers in Class of 1942 Professor of Chemistry Matthew D. Shoulders’ lab have uncovered a sinister hidden mechanism that can allow cancer cells to survive (and, in some cases, thrive) even when hit with powerful drugs. The secret lies in a cellular “safety net” that gives cancer the freedom to develop aggressive mutations.
This fascinating intersection between molecular biology and evolutionary dynamics, published today on the cover of Molecular Cell, focuses on the most famous anti-cancer gene in the human body, TP53 (tumor protein 53, known as p53), and suggests that cancer cells don’t just mutate by accident—they create a specialized environment that makes dangerous mutations possible.
The Guardian Under Attack
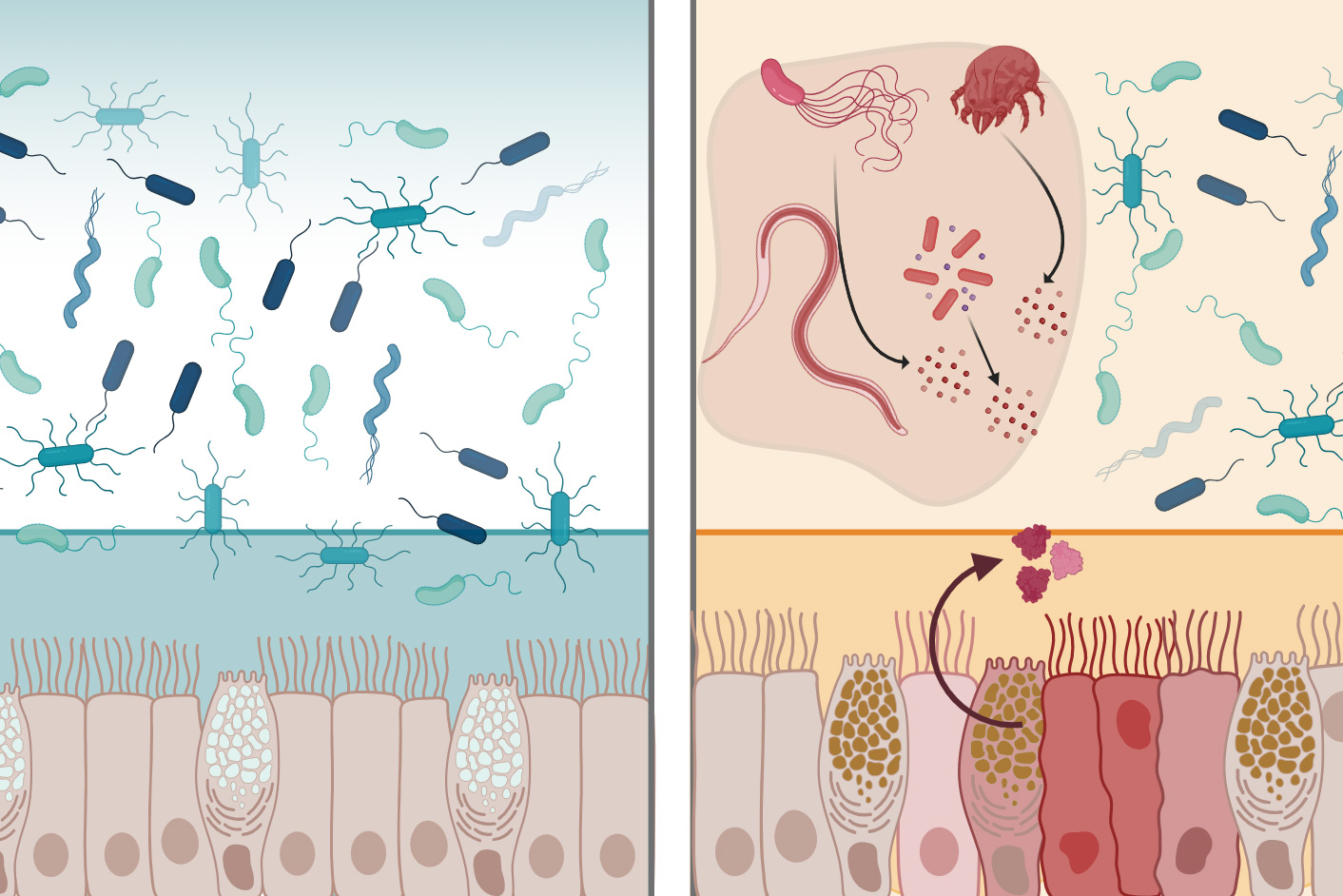
Tasked with the job of stopping damaged cells from dividing, the p53 protein has been known for decades as the “guardian of the genome” and is the most mutated gene in cancer. Some of the most perilous of these mutations are known as “dominant-negative” variants. Not only do they stop working, but they actually prevent any healthy p53 in the cell from doing its job, essentially disarming the body’s primary defense system.
A Chaperone for Bad Behavior
To function, p53 and most other proteins must fold into specific 3D shapes, much like precise cellular origami. Typically, if a mutation occurs that ruins this shape, the protein becomes a tangled mess, and the cell destroys it.
A specialized network of proteins, called cellular chaperones, help proteins fold into their correct shape, collectively known as the proteostasis network.
“Many chaperone networks are known to be upregulated in cancer cells, for reasons that are not totally clear,” said Stephanie Halim, a graduate student in the Shoulders Group and co-first author of the study along with Rebecca Sebastian (PhD ‘22), an alumnus of the Shoulders Group. “We hypothesized that increasing the activities of these helpful protein folding networks can allow cancer cells to tolerate more mutations than a regular cell.”
The research team investigated a “helper” system in the cell called the proteostasis network. This network involves many proteins known as chaperones that help other proteins fold correctly. A master regulator called Heat Shock Factor 1 (HSF1) controls the composition of the proteostasis network, with HSF1 activity upregulating the network to create supportive protein folding environments in response to stress. In healthy cells, HSF1 stays dormant until heat or toxins appear. In cancer, HSF1 is often permanently in action mode.
To see how this works in real-time, the team created a specialized cancer cell line that let them chemically “turn up” the activity of HSF1 on demand. They then used a cutting-edge technique to express every possible singly mutated version of a p53 protein—testing thousands of different genetic “typos” at once.
The results were clear: when HSF1 was amplified, the cancer cells became much better at handling “bad” mutations. Normally, these specific mutations are so physically disruptive that they would cause the protein to collapse and fail. However, with HSF1 providing extra folding help, these unstable, cancer-driving proteins were able to stay intact and keep the cancer growing.
“These findings show that chaperone networks can reshape the fundamental mutational tolerance of the most mutated gene in cancer, linking proteostasis network activity directly to cancer development,” said Halim. “This work also puts us one step closer to understanding how tinkering with cellular protein folding pathways can help with cancer treatment.”
Unravelling Cancer’s Safety Net
The study revealed that HSF1 activity specifically protects normally disruptive amino acid substitutions located deep inside the protein’s core—the most sensitive areas. Without this extra folding help, these substitutions would likely cause degradation of these proteins. With it, the cancer cell can keep these broken proteins around to help it grow.
This discovery helps explain why cancer is so resilient, and why previous attempts to treat cancer by blocking chaperone proteins (like HSP90, an abundant cellular chaperone) have been so complex. By understanding how cancer “buffers” its own bad mutations, doctors may one day be able to break that safety net, forcing the cancer’s own mutations to become its downfall.
The research was conducted in collaboration with the labs of Professor Yu-Shan Lin (Tufts University), Professor Francisco J. Sánchez-Rivera (MIT Department of Biology), Professor William C. Hahn (Institute Member of the Broad Institute and Professor of Medicine in the Department of Medical Oncology at the Dana-Farber Cancer Institute and Harvard Medical School), and Professor Marc L. Mendillo (Northwestern University).