A new way to reprogram immune cells and direct them toward anti-tumor immunity
MIT scientists’ discovery yields a potent immune response, could be used to develop a potential tumor vaccine.
A collaboration between four MIT groups, led by principal investigators Laura L. Kiessling, Jeremiah A. Johnson, Alex K. Shalek, and Darrell J. Irvine, in conjunction with a group at Georgia Tech led by M.G. Finn, has revealed a new strategy for enabling immune system mobilization against cancer cells. The work, which appears today in ACS Nano, produces exactly the type of anti-tumor immunity needed to function as a tumor vaccine — both prophylactically and therapeutically.
Cancer cells can look very similar to the human cells from which they are derived. In contrast, viruses, bacteria, and fungi carry carbohydrates on their surfaces that are markedly different from those of human carbohydrates. Dendritic cells — the immune system’s best antigen-presenting cells — carry proteins on their surfaces that help them recognize these atypical carbohydrates and bring those antigens inside of them. The antigens are then processed into smaller peptides and presented to the immune system for a response. Intriguingly, some of these carbohydrate proteins can also collaborate to direct immune responses. This work presents a strategy for targeting those antigens to the dendritic cells that results in a more activated, stronger immune response.
Tackling tumors’ tenacity
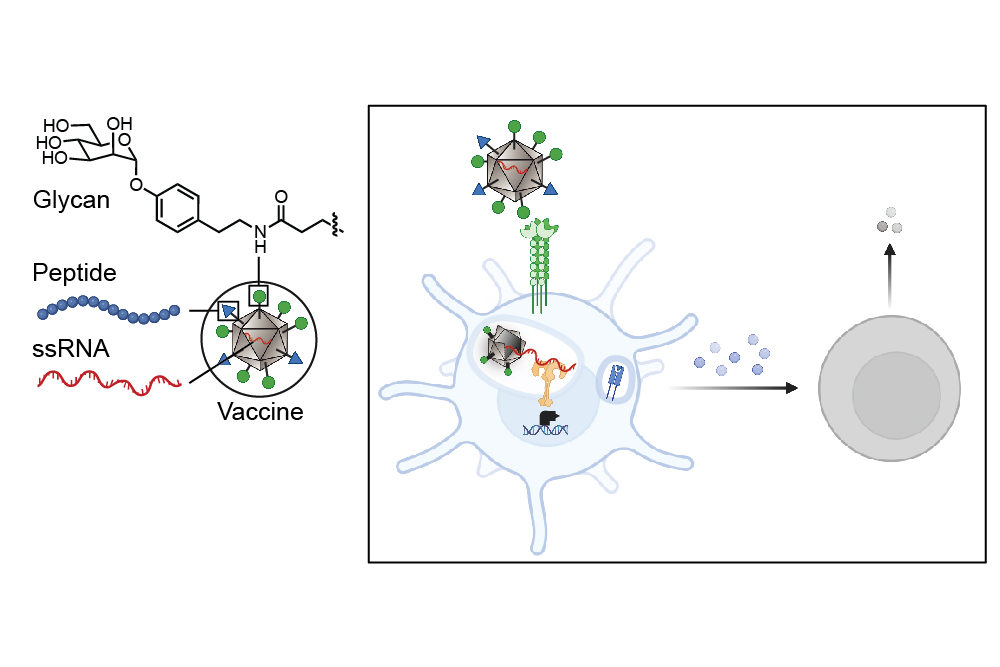
The researchers’ new strategy shrouds the tumor antigens with foreign carbohydrates and co-delivers them with single-stranded RNA so that the dendritic cells can be programmed to recognize the tumor antigens as a potential threat. The researchers targeted the lectin (carbohydrate-binding protein) DC-SIGN because of its ability to serve as an activator of dendritic cell immunity. They decorated a virus-like particle (a particle composed of virus proteins assembled onto a piece of RNA that is noninfectious because its internal RNA is not from the virus) with DC-binding carbohydrate derivatives. The resulting glycan-costumed virus-like particles display unique sugars; therefore, the dendritic cells recognize them as something they need to attack.
“On the surface of the dendritic cells are carbohydrate binding proteins called lectins that combine to the sugars on the surface of bacteria or viruses, and when they do that they penetrate the membrane,” explains Kiessling, the paper’s senior author. “On the cell, the DC-SIGN gets clustered upon binding the virus or bacteria and that promotes internalization. When a virus-like particle gets internalized, it starts to fall apart and releases its RNA.” The toll-like receptor (bound to RNA) and DC-SIGN (bound to the sugar decoration) can both signal to activate the immune response.
Once the dendritic cells have sounded the alarm of a foreign invasion, a robust immune response is triggered that is significantly stronger than the immune response that would be expected with a typical untargeted vaccine. When an antigen is encountered by the dendritic cells, they send signals to T cells, the next cell in the immune system, to give different responses depending on what pathways have been activated in the dendritic cells.
Advancing cancer vaccine development
The activity of a potential vaccine developed in line with this new research is twofold. First, the vaccine glycan coat binds to lectins, providing a primary signal. Then, binding to toll-like receptors elicits potent immune activation.
The Kiessling, Finn, and Johnson groups had previously identified a synthetic DC-SIGN binding group that directed cellular immune responses when used to decorate virus-like particles. But it was unclear whether this method could be utilized as an anticancer vaccine. Collaboration between researchers in the labs at MIT and Georgia Tech demonstrated that in fact, it could.
Valerie Lensch, a chemistry PhD student from MIT’s Program in Polymers and Soft Matter and a joint member of the Kiessling and Johnson labs, took the preexisting strategy and tested it as an anticancer vaccine, learning a great deal about immunology in order to do so.
“We have developed a modular vaccine platform designed to drive antigen-specific cellular immune responses,” says Lensch. “This platform is not only pivotal in the fight against cancer, but also offers significant potential for combating challenging intracellular pathogens, including malaria parasites, HIV, and Mycobacterium tuberculosis. This technology holds promise for tackling a range of diseases where vaccine development has been particularly challenging.”
Lensch and her fellow researchers conducted in vitro experiments with extensive iterations of these glycan-costumed virus-like particles before identifying a design that demonstrated potential for success. Once that was achieved, the researchers were able to move on to an in vivo model, an exciting milestone for their research.
Adele Gabba, a postdoc in the Kiessling Lab, conducted the in vivo experiments with Lensch, and Robert Hincapie, who conducted his PhD studies with Professor M.G. Finn at Georgia Tech, built and decorated the virus-like particles with a series of glycans that were sent to him from the researchers at MIT.
“We are discovering that carbohydrates act like a language that cells use to communicate and direct the immune system,” says Gabba. “It’s thrilling that we have begun to decode this language and can now harness it to reshape immune responses.”
“The design principles behind this vaccine are rooted in extensive fundamental research conducted by previous graduate student and postdoctoral researchers over many years, focusing on optimizing lectin engagement and understanding the roles of lectins in immunity,” says Lensch. “It has been exciting to witness the translation of these concepts into therapeutic platforms across various applications.”